Treating a stubborn blood disease that strikes children may come down to tweaking energy production in stem cells, suggests research out of West Virginia University.
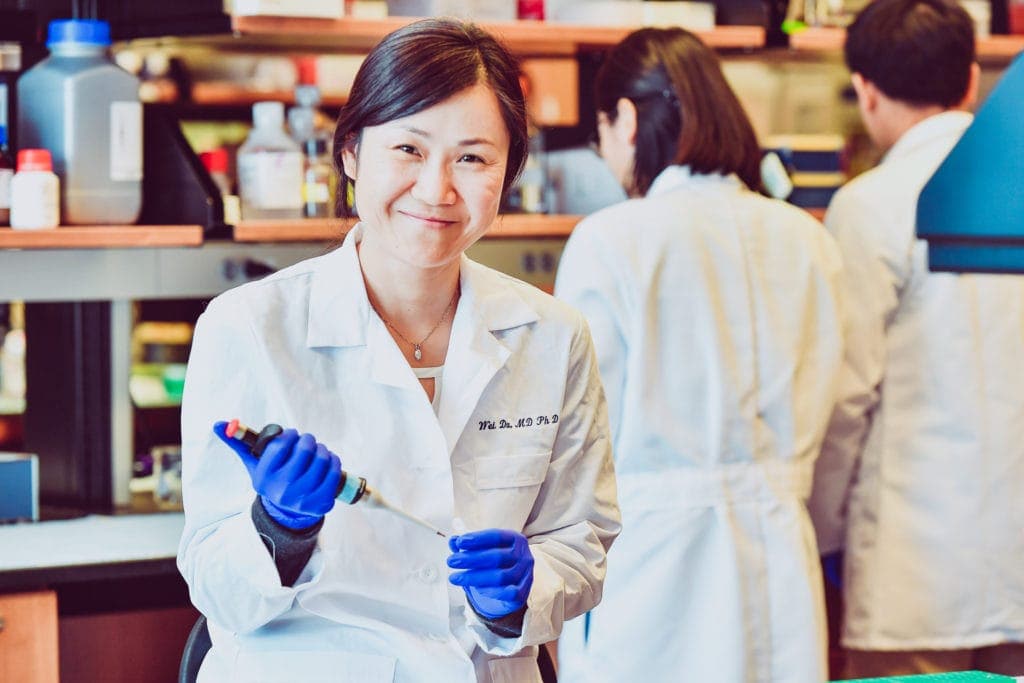
Wei Du, an assistant professor in the School of Pharmacy, is investigating the link between how stem cells make energy and how Fanconi anemia develops. The disease makes it harder for bone marrow to churn out the blood cells our bodies need to fight illnesses, stanch bleeding and transport oxygen. It also makes repairing damaged DNA more difficult.
“Almost all of the kids with Fanconi anemia will develop leukemia eventually,” said Du, who co-leads the Alexander B. Osborn Hematopoietic Malignancy and Transplantation Program at the WVU Cancer Institute. According to St. Jude Children’s Research Hospital, the average lifespan for people with the disease is between 20 and 30 years.
Du and her research team discovered that, in animal models of Fanconi anemia, stem cells tended to use aerobic—or oxygen-based—processes to make energy. That’s unusual: normally stem cells found in bone marrow and blood prefer an anaerobic process that doesn’t rely on oxygen.
This metabolic distinction suggests that Fanconi anemia’s diverse symptoms—from fatigue and shortness of breath, to frequent bruising and nosebleeds—may hinge on cellular-level energy production.
In fact, a single step in the metabolic process seems crucial. The researchers identified a specific signaling pathway—called the p53-TIGAR axis—that was overexpressed in the anemic models. The overexpression correlated to the aerobic “rerouting” of the stem cells’ energy production.
The current standard of care for Fanconi anemia includes bone marrow transplant, but as Du explained, it works less than one-third of the time. “In people with Fanconi anemia, blood cells aren’t the only ones that have a mutation,” she said. “So do other cells in other parts of the body that support stem cell survival.” For that reason, the patients’ bodies can’t support the replication of healthy, transplanted normal cells properly, and their anemia persists.
But Du’s findings could lead to new and better treatments for Fanconi anemia. One promising option is a drug that inhibits the overactivation of the p53-TIGAR signal. Preventing p53-TIGAR from inordinate activation may guide the stem cells’ energy production back to the usual pathway.
Her insights might even deepen researchers’ understanding of gene-therapy techniques. “If you know more about diseases of the stem cell—how they regulate energy, and how they regulate differentiation and self-renewal—you probably can improve gene therapy as well,” Du said. “If you can manually balance the energy production of the diseased stem cells then maybe this can be a benefit when you harvest those gene-delivery cells and transplant them into the patient.”
Wei Du’s work is supported by the National Institutes of Health under Award Number P20GM121322, a Leukemia Research Foundation grant and an American Cancer Society grant. The findings and conclusions in this article are solely those of the authors and do not necessarily represent the official position of the funding agencies.